We all acknowledge that food impacts our physical health, but emerging evidence suggests it can shape our mental health also, spawning a new field of science known as nutritional psychiatry.
Though the field is still in its infancy, research suggests that adherence to a Mediterranean diet reduces your risk of depression and cognitive decline.
Parallel to this, studies broadly show that a Western diet high in fried foods, refined grains and saturated fats is positively associated with an increased risk of cognitive decline and depression.
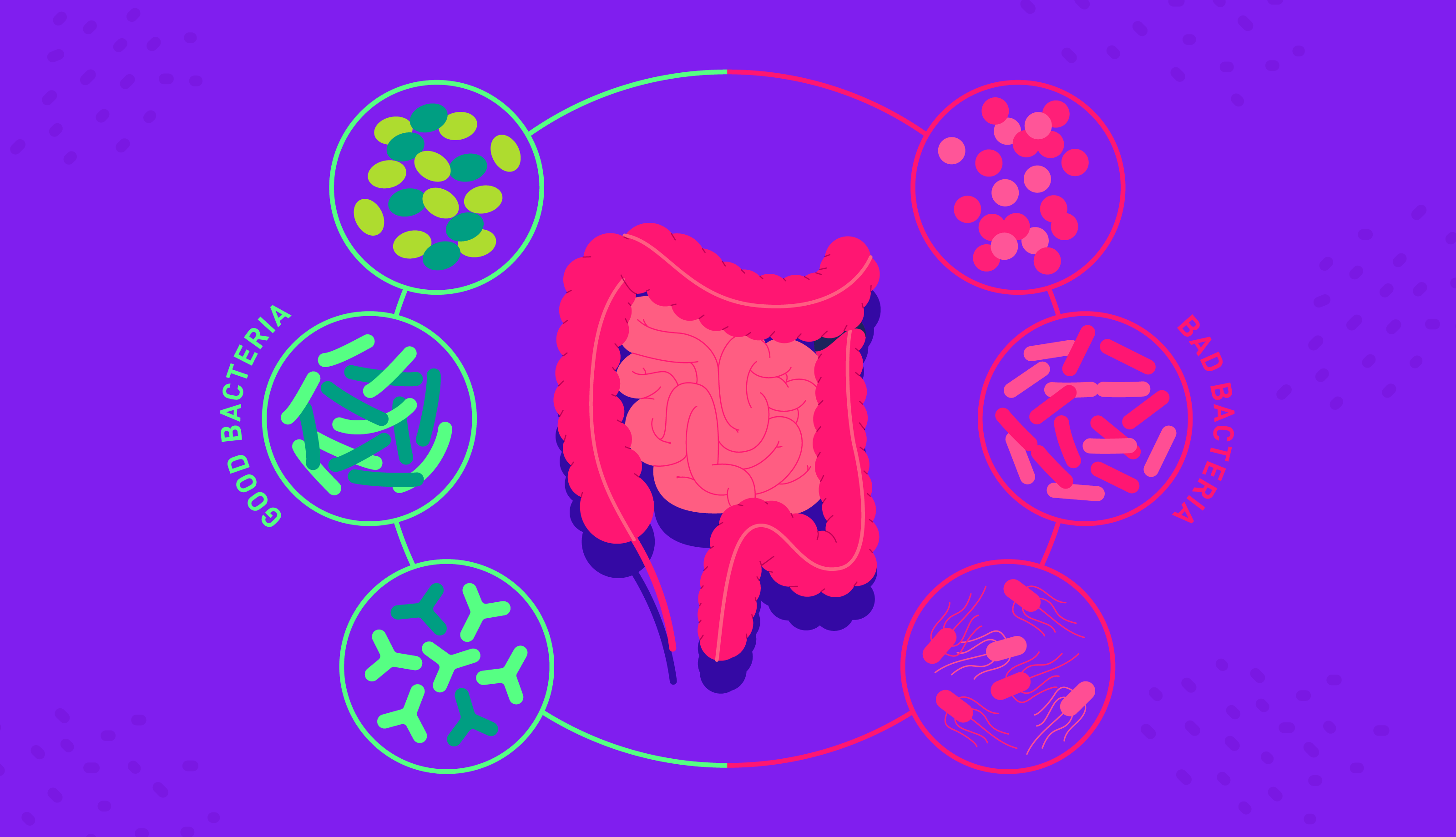
Multiple biological pathways have been suggested for how food can influence mood, prime among them the gut microbiome. Other potential mechanisms include oxidative stress, low-grade chronic inflammation and blood sugar spikes.
Table of contents
- Nutritional Psychiatry
- Which diet is best for mental health?
- How does food affect mood?
- Diet, inflammation and the microbiome
- Oxidative stress and neuroplasticity
- Glycemic index and blood sugar spikes
- Food for feelings: summary
Nutritional Psychiatry

Nutritional psychiatry is an emerging field that seeks to address mental health issues through diet. The discipline is founded upon a robust and compelling body of evidence that suggests specific dietary patterns can improve mental health and reduce the risk of mood disorders.
A prominent figure in this movement is Felice Jacka, director of the Food and Mood Centre at Deakin University and president of the Society for Nutritional Psychiatry.
Jacka’s studies culminated in a PhD paper that compared the levels of anxiety and depression among women following a traditional diet (high in vegetables, fish, fruits, nuts and whole grains) and those on a typical Western diet characterised by fried foods, refined grains and processed goods.
In light of the research to date, an overview paper published by the Nutrition Society concluded that nutritional psychiatry is “a rapidly growing field of research that has the potential to provide clinically meaningful interventions to both prevent and manage mental illness.”
☝TOP TIP☝ When you take an Atlas Microbiome Test, you’ll discover your microbiome enterotype. Your enterotype reflects your long-term dietary habits and can suggest whether you are following a Western Diet or a more traditional one.
Which diet is best for mental health?

Numerous studies have examined the impact of dietary interventions on mental health, most of which are observational.
Collectively, their results strongly suggest that nutrition can cause meaningful changes in mood and potentially reduce depressive symptoms.
Independent of exercise or lifestyle factors, traditional nutritional practices such as a Mediterranean and Japanese diet have been shown to reduce the risk of depression by as much as 30%.
Likewise, a study published in the American Journal of Clinical Nutrition performed a systematic review and meta-analysis of 13 studies looking at the impact of diet on mental health.
Based on the results, the researchers concluded that a high intake of whole grains, fruit, vegetables and fish might be associated with a reduced risk for depression. The Mediterranean diet shows particular promise as a dietary intervention for mood disorders.
Inspired by the eating patterns of those around the Mediterranean sea, the diet is rich in whole grains, fruits, vegetables, legumes, nuts and healthy fats such as olive oil and omega 3.
As such, it is packed full of vitamins B and D alongside cognitive-boosting nutrients like selenium, iron, folate, fibre and omega 3.
In observational and preliminary clinical studies, the Mediterranean diet has been consistently associated with reduced cognitive decline and depression risk.
For example, the Annals of Neurology published a meta-analysis of 22 papers exploring the effect of a Mediterranean diet on depression and cognitive impairment.
The study found that both a high and moderate adherence to the diet was associated with reduced cognitive decline and risk of depression.
Long-term studies with bigger cohorts have reached similar conclusions; a four-year longitudinal study following over 10,000 Spanish students found that adherence to the Mediterranean diet is potentially protective against depressive disorders.
The first high-quality study to investigate the impact of the Mediterranean diet on mood was the so-called SMILES trial.
The single-blind, randomised controlled trial ran from 2012 to 2015 and sought to rigorously measure the effect of the Mediterranean diet on depressive symptoms.
Sixty-seven participants enrolled in the trial, all of whom suffered from moderate to severe depression. Of this group, 33 participants received nutritional counselling and followed a modified Mediatarenean diet for 12 weeks. The remaining 37 participants received social support, meaning they met weekly with the research team.
By the end of twelve weeks, the dietary support group showed significantly more improvement in depressive symptoms than their counterparts, with 32.8% achieving remission compared to 8% of the control group.
The results suggest that dietary intervention could be an effective and accessible way to treat depression, though more high-quality trials are needed to confirm these results.
Better still, the Mediterranean diet has been linked with an impressive list of health benefits, including a reduced risk of coronary heart disease, cancers, stroke and all-cause mortality.
☝FUN FACT☝ 20% of everything you eat goes to the brain!
How does food affect mood?
Researchers have suggested multiple viable mechanisms for how food can influence mood, including changes in the gut microbiome, blood sugar spikes, oxidative stress and low-grade chronic inflammation.
Diet, inflammation and the microbiome
Observational studies have noted a higher prevalence of inflammation in conditions such as bipolar disorder and depression, suggesting there may be a link between the two.
An imbalance in the microbiome can compromise the gut lining, allowing bacteria to enter the blood via the gut and trigger inflammatory cells. Colloquially known as “leaky gut”, increased permeability can lead to low-grade chronic inflammation in the bowel and beyond.

There are lots of risk factors for dysbiosis, including stress, excessive antibiotic use and most importantly, poor diet.
In particular, a diet high in saturated fats and refined sugars can deplete the microbiome of butyrate, an anti-inflammatory short-chain fatty acid that strengthens the gut lining.
By putting the pieces together, researchers theorise that a Western diet can deplete the microbiome of beneficial bacteria, weakening the gut lining and increasing inflammation.
In turn, It is thought that pro-inflammatory cells can travel throughout the body and penetrate the blood-brain barrier, impacting mood and behaviour.
Animal studies further reinforce the link between the microbiome and depression; for example, when researchers transplant the poo of those with manic depression into mice, the rodents begin exhibiting depressive behaviours.
Oxidative stress and neuroplasticity
Oxidative stress occurs when there is an imbalance between unstable free radicals and detoxifying antioxidants in the body.
The phenomenon has been linked with cancer, heart disease, and, you guessed it, depression; both animal and human studies have shown that those with depression have elevated levels of oxidative stress compared to healthy controls.
Unsurprisingly, a Western diet is associated with the condition, whilst a Mediterranean diet, rich in antioxidant fruit and vegetables, is linked with reduced DNA damage due to free radicals.
Our brains are plastic, meaning they can change shape and structure in response to experiences throughout life. Emerging research suggests that dietary choices may be able to physically alter the size of the hippocampus, a brain region that is central to learning, memory and mood.
One of the main drivers behind neuroplasticity is a protein called brain-derived neurotrophic factor (BDNF). In short, BDNF plays a crucial role in the growth of nerve cells. Intriguingly, the protein is seen at lower levels in individuals with depression.
Although the research is scarce, a study following 250 women aged 60 has shown that low intake of nutrient-dense foods and high adherence to the Western diet is associated with decreased volume in the left hippocampal lobe.
Likewise, a longitudinal study looking at over 450 individuals also found that long-term healthy diet quality was associated with a larger total hippocampal volume.
☝TOP TIP☝ With an Atlas Microbiome Test, you’ll receive weekly, personalised dietary recommendations to boost butyrate-producing bacteria and encourage microbiome diversity. You will also uncover the inflammatory potential of your microbiome based on its diversity and composition.
Glycemic index and blood sugar spikes
Glycemic Index (GI) measures how quickly your body breaks down carbohydrates into glucose, whilst Glycemic Load (GL) measures how much glucose per serving a portion of food can deliver.
If food is low GI, it takes your body longer to metabolise the carbohydrate, resulting in a gradual rise in blood sugar levels. On the contrary, high GI and GL foods, such as refined carbs and sugary snacks, lead to a drastic rise in blood sugar levels.
As we all know, what goes up must come down, and when glucose levels crash, it can result in fatigue, irritability, depression and anxiety.
Generally, many foods prominent in a Mediterranean diet, such as legumes and whole grains, are low to moderate GI. As such, they keep you fuller for longer and stabilise blood sugar levels.
On the other hand, the Western diet contains many high GI foods that can cause a rollercoaster of glucose spikes and crashes.
Worse still, these peaks and troughs can lead to mood swings and intense cravings for sugary snacks. Blood sugar related mood swings offer another pathway through which diet can impact mental health.
Food for thought: summary
Numerous observational studies suggest that specific dietary patterns can influence mood; most notably, the Mediterranean diet has been consistently associated with a reduced risk for depression, cognitive decline and low mood.
Firstly, a diet rich in prebiotic fibre, legumes, nuts and whole grains can enrich the microbiome with beneficial bacteria.
In particular, many of these food types encourage the production of butyrate-producing bacteria, a short-chain fatty acid that strengthens the gut lining and prevents inflammation.
Secondly, the Mediterranean diet is rich in vitamins and minerals which can boost mood, including iron, folate and vitamin B12. All of these nutrients play a role in the production of serotonin, also known as the “happy hormone”.
Likewise, the Mediterranean diet contains many antioxidant compounds that can reduce oxidative stress, a condition observed in numerous mood disorders.
Lastly, plant-based fibre and whole grains generally have a low GI and GL, meaning they are broken down into glucose gradually in the body.
As such, these foods can help stabilise blood sugar levels and prevent spikes- and crashes- along with associated mood swings.
Whilst nutritional psychiatry should not replace traditional therapies for mood disorders, namely antidepressants and cognitive behavioural therapy, it should not be ignored either.
Evidence suggests that what we put in our mouths can change our mental well-being for better or worse. In light of this, food should be seriously considered as a complementary or alternative treatment for mood disorders.
What's more, the eating patterns associated with improved mood also benefit physical health. For example, a Mediterranean diet is associated with a reduced risk for certain cancers, heart disease, obesity, and all-cause mortality. With this in mind, there is no reason not to transition to this way of eating.
☝️DISCLAIMER☝This article is for informational purposes only. It is not intended to constitute or be a substitute for professional medical advice, diagnosis, or treatment.