Evidence suggests that intermittent fasting can improve cardiovascular and metabolic health, potentially helping to manage type-2 diabetes. We explore the benefits and risks of intermittent fasting, including how it impacts the gut microbiome.
Table of contents
- What is intermittent fasting?
- Methods of intermittent fasting
- Benefits of intermittent fasting
- Metabolic reprogramming
- Weight loss and hormonal changes
- Can Intermittent fasting help manage type-2 diabetes?
- Fasting and the gut microbiome
- Who should avoid intermittent fasting?
- Article summary
What is intermittent fasting?

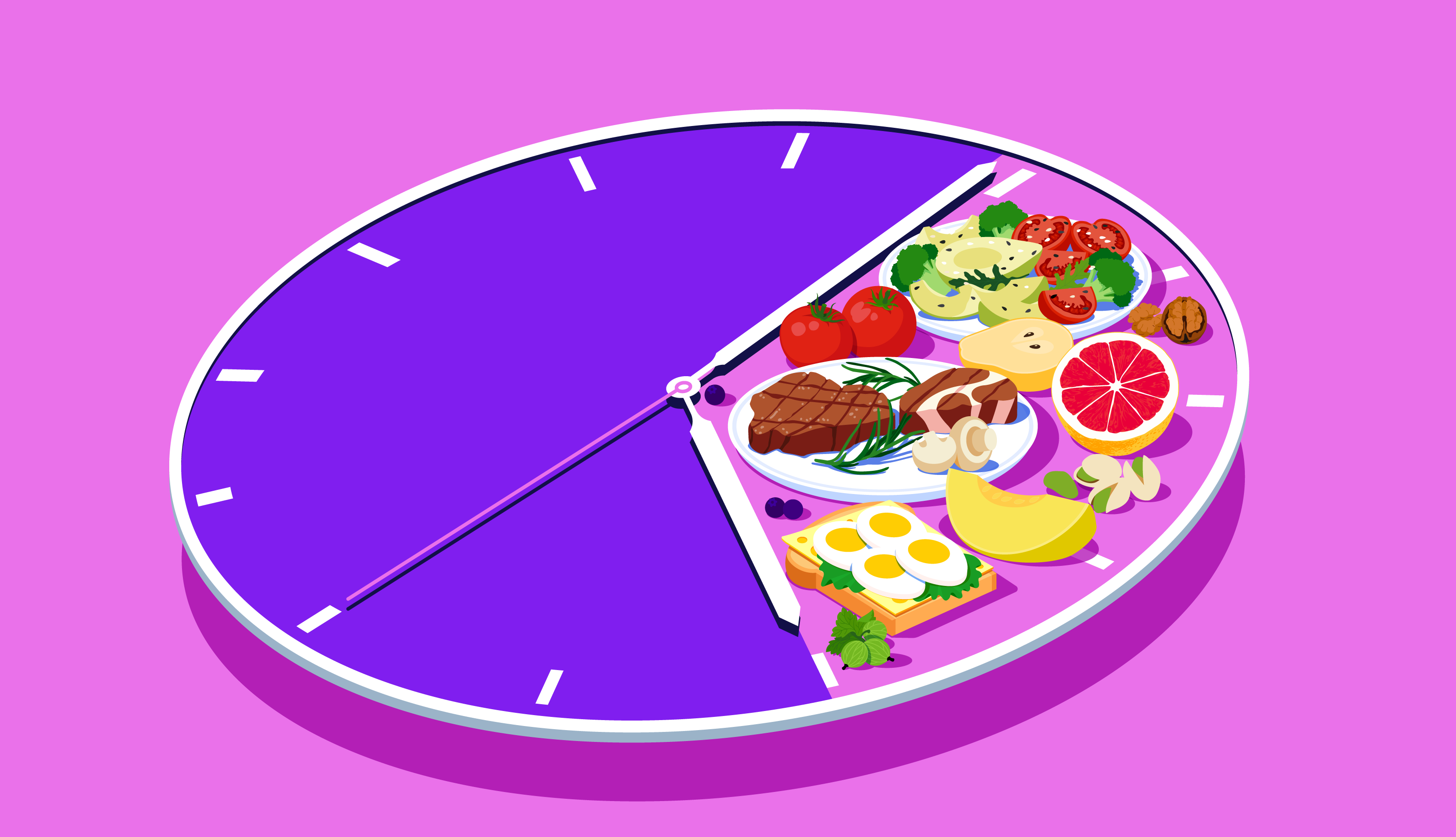
Intermittent fasting refers to any eating plan where you alternate between periods of eating normally and fasting.
All of us naturally fast when we sleep; however, intermittent fasting is a conscious decision to not eat (or drastically restrict calorie intake) over a given period, be that hours or days.
Intermittent fasting was highly popularised by Dr Michael Mosely with his book the Fast 800 alongside his hit BBC documentary, Eat, Fast, Live Longer.
Strictly speaking, intermittent fasting only tells you when to eat, not what to eat. However, common fasting plans often recommend certain diets, such as the DASH or Mediterranean, during feeding periods.
Methods of intermittent fasting
There are three primary methods of intermittent fasting, including alternate-day fasting, daily time-restricted fasting and the 5:2 plan, explained in the table below:
The 5:2 method: This plan involves eating your normal diet five days a week and then restricting your intake to around 600-800 calories for two days of your choosing. The fasting days are generally not consecutive.
Daily time-restricted fasting: This method involves eating during select "windows" of time each day and then fasting outside of these.
The most popular iteration is the 16:8 method, in which you fast for 16 hours and eat for 8. For example, you might eat from 9 am to 5 pm and then fast from 5 pm until 9 am.
Alternate-day fasting: The basic idea behind alternate-day fasting is that you eat what you want on one day and then fast on the next, repeating the process. The plan splits the week evenly between days of fasting and those eating normally.
Benefits of intermittent fasting
Findings from animal and human research suggest intermittent fasting can improve cardiovascular health, lowering BMI, cholesterol levels and blood pressure.
For example, one study found that intermittent fasting coupled with the Dietary Approaches to Stop Hypertension (DASH) diet reduced weight and blood pressure significantly more than the dietary intervention alone.
Simultaneously, intermittent fasting has also been shown to help regulate blood sugar levels and reduce inflammation, independent of weight loss.
The reigning hypothesis states that intermittent fasting can confer these benefits via two main mechanisms; reducing inflammation and "reprogramming" your metabolism, changing how your body stores and sources energy. Let me explain.
☝Fun fact☝ Paracelsus, one of the fathers of modern medicine, is quoted as saying "Fasting is the greatest remedy- the physician within".
Metabolic reprogramming

In a "fed" state, your body sources energy from glucose- beginning with the circulating glucose and turning to stored glycogen soon after.
Once glycogen stores are depleted, the body undergoes a "metabolic switch", swapping from glucose as its primary energy source to ketones in fatty tissue.
How long it takes to enter ketosis will vary depending on the meal you ate, genetics and activity levels, though on average, it occurs between 12-24 hours after eating.
Autophagy can produce new, healthier cell structures and enhance the body's ability to neutralise free radicals.
According to a review study written by researchers at the National Institute Of Ageing, metabolic reprogramming may protect against cognitive decline too.
We don't have any studies to demonstrate this in humans, but alternate day fasting has been observed to slow cognitive decline in mice predisposed to Alzheimer's (check out the video above).
Once the metabolic switch has been triggered, the benefits carry over to a non-fasting state, improving glucose regulation, increasing stress resistance and reducing inflammation.
Weight loss and hormonal changes
Adipose tissue (body fat) produces and releases hormones, which can either be inflammatory (leptin) or anti-inflammatory (adiponectin).
Multiple studies show that intermittent fasting can reduce weight, particularly in obese individuals, although it remains unclear whether it is more effective than a normal, calorie-restricted diet.
Fasting-related weight loss not only reduces adipose tissue, it also triggers chemical changes that can have beneficial effects throughout the body.
More specifically, intermittent fasting has been shown to reduce leptin (a fullness hormone) and increase the levels of adiponectin, low levels of which are associated with obesity and insulin resistance.
A systematic review and meta-analysis comparing an intermittent fasting diet with a control diet found that IF reduced blood glucose and BMI, which corresponded to a reduction in leptin levels and an increase in adiponectin.
Researchers suspect that obesity and metabolic disorders may partly result from leptin resistance, which would explain why these demographics often exhibit high levels of this satiety hormone.
Can Intermittent fasting help manage type-2 diabetes?

Type-2 diabetes is thought to arise due to insulin resistance and dysfunctions in insulin production.
Treatment often involves injecting insulin each day, although, over time, this may worsen insulin resistance.
As we have discussed, IF may be able to increase insulin sensitivity and regulate blood sugar levels, making it an attractive treatment option for those with type-2 diabetes.
The TV presenter and health author Dr Michael Mosely claims he reversed his type-2 diabetes and lost 10kg using the 5:2 fasting method in combination with a Mediterranean diet.
Likewise, a case series published in the British Medical Journal followed three diabetic patients on a fasting regime over three months (24 hours fast, three days a week).
All three participants saw significant reductions in blood glucose levels and weight, discontinuing their insulin medication after one month.
Whilst compelling, case reports rank low on the hierarchy of evidence, although they can suggest new avenues for clinical research. So what does the available evidence suggest regarding intermittent fasting and diabetes?
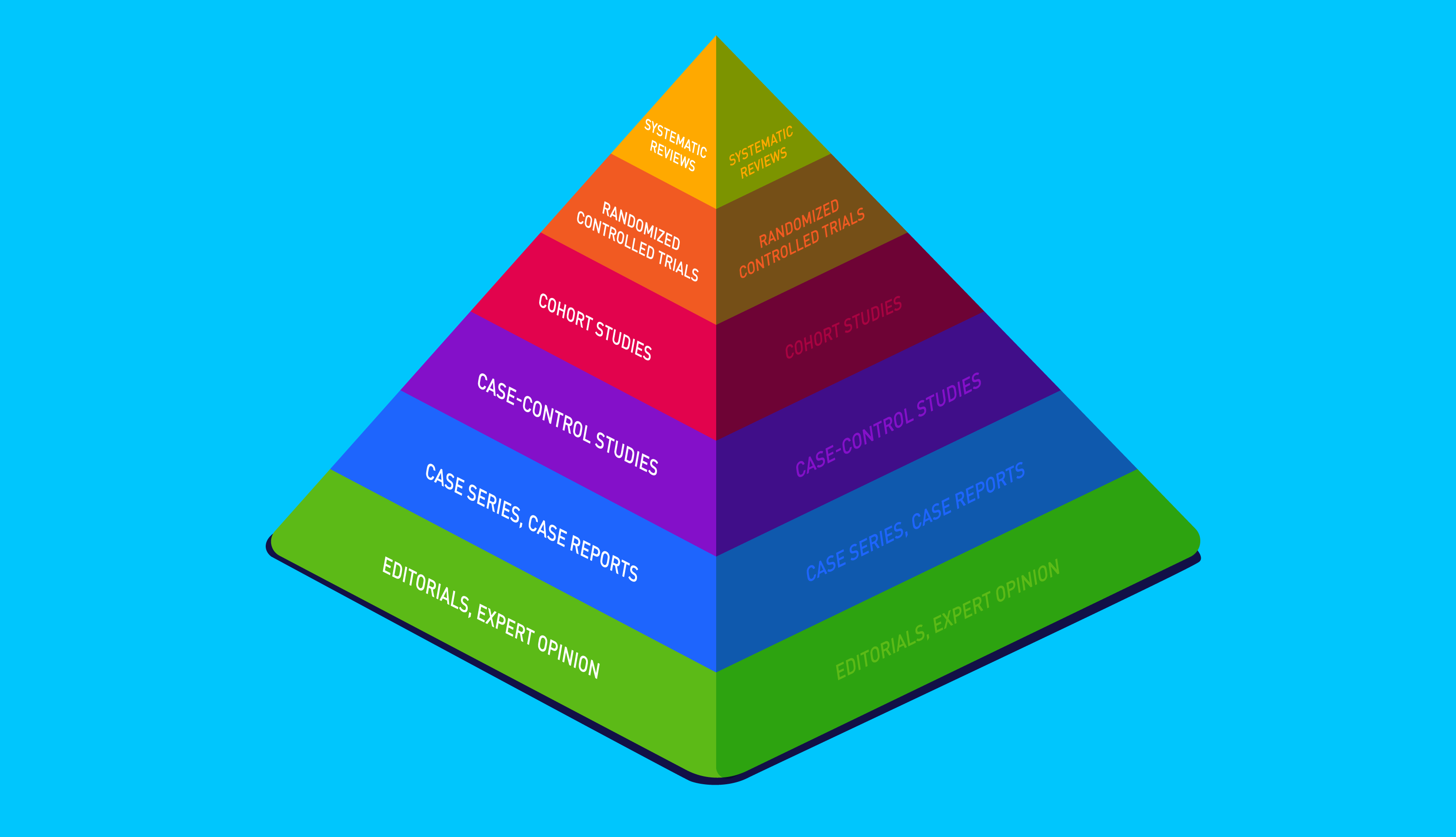
A paper published in the Journal Of Clinical Diabetes And Endocrinology summarised the scientific literature on IF and type-2 diabetes to date, seeking to establish whether IF has therapeutic potential for the condition.
Based on 17 studies, including 2 case reports and 15 clinical trials, the paper suggests that intermittent fasting may be a viable treatment for type-2 diabetes (not type-1), provided it's overseen by a medical professional.
On the balance of evidence, the study concludes that IF may be able to improve insulin sensitivity via metabolic reprogramming and by reducing visceral fat.
These findings are paralleled by a systematic review and meta-analysis, which looked at 12 studies, all comparing an intermittent fasting diet (IFD) with a regular/calorie-restricted diet.
Compared to controls, the IFD was significantly associated with lower weight and blood sugar levels, likely mediated by an increase in adiponectin.
Lastly, a systematic review and meta-analysis of 7 studies found that intermittent fasting is linked with greater weight reduction than a standard diet (1.8kg on average), but did not affect blood sugar levels.
Whilst intermittent fasting may be able to help some individuals with diabetes, diabetics are at an elevated risk for hypoglycemia (low blood glucose levels) when fasting, especially when taking insulin and other medications.
☝IMPORTANT☝ If you want to try and manage type-2 diabetes with a fasting regime, consult your doctor beforehand. It is important to monitor your blood glucose levels during the process to avoid complications.
Fasting and the gut microbiome

In rodents, time-restricted feeding has been shown to increase the production of short-chain fatty acids, boost microbial diversity and minimise inflammation.
The research on how intermittent fasting impacts the human microbiome is scarce, with the papers available few in number and small in scale.
Early research suggests that fasting may alter the microbiome in beneficial ways, increasing diversity and reinforcing the intestinal wall.
In one study, 13 overweight men and women were asked to follow an extremely low-calorie diet (600-800 calories) for seven days, the same amount of calories allowed on fasting days during the 5:2 regime.
Poo samples were taken before and after the study, allowing the team to measure changes in the microbiome.
The fasting week triggered noticeable microbiome composition shifts, increasing overall microbiome diversity and enrichment in Akkermansia and Bifidobacteria species across the study group.
Akkermansia is a unique bacteria that feed on the mucus in your gut lining, a little bit like the fish you see in spars that nibble away at the dead skin on your feet.
As they feed on the gut lining, Akkermansia stimulates the growth of new cells, strengthening the intestinal barrier and minimising inflammation. Akkermansia can also cross-feed other beneficial bacteria, such as Firmicutes species, with their metabolites.
So how do other fasting plans impact the microbiome, such as the 16:8 method?
A team of researchers at Nanjing medical university put this to the test. They recruited 80 healthy young males, 56 of whom followed a 16:8 fasting regime for 25 days, while the remainder ate normally.
After 25 days, the IF group showed increased microbial richness and enrichment in Prevotellaceae and Bacteroideaceae. Parallel to this, they experienced a downregulation of inflammatory genes and reduced cholesterol levels.
Before you get too excited, another pilot study trialled the 16:8 method in obese men over 12 weeks; interestingly, they witnessed no changes in microbiome composition or diversity, although the subjects did lose weight during the intervention.

During the holy month of Ramadan, Muslims fast from sunrise to sunset for a month. Depending on where they are in the world, the fasting period can last anywhere from 10-19 hours (a form of daily time-restricted eating).
Several studies have shown that Ramadan fasting can confer health benefits in some groups, including increased microbial richness and reduced cholesterol.
In one study published in the American Journal Of Nutrition, males fasting 16 hours daily for Ramadan experienced significant shifts in their microbiome composition, including enrichment in the butyrate-producing species Lachnospiraceae.
Considering this bacterial species is associated with a reduced risk for cancer and inflammatory bowel disease, the researchers hypothesise that it may modulate the beneficial effects of intermittent fasting on human health (reduced blood sugar and cholesterol). However, further research is needed to confirm the hypothesis.
The study was split into a younger and a middle-aged cohort. Interestingly, the younger participants showed statistically significant increases in microbiome diversity, considered a broad marker of health.
On the contrary, the middle-aged cohort showed no such increase in diversity. It is well known that ageing naturally reduces microbial diversity, which may partly account for these results. After Ramadan, the microbiome composition returned to normal in both groups.
Moroever, a pilot study following nine subjects during Ramadan observed significant compositional changes to the microbiome.
In particular, the participants saw an enrichment in several beneficial species, including butyrate-producing Faecalibacterium and Roseburia, with the greatest enrichment in Butyricicoccus pullicaecorum.
Like Akkermanisa, B. pullicaecorum is one of a few bacterial species that feeds on mucus in the gut lining. These little architects can reinforce the gut wall and combat inflammation.
Lastly, a paper published in Food Microbiology compared the microbiomes of two cohorts undergoing fasting for Ramadan, including a Chinese and Pakistani group.
Both groups saw shifts in their microbiome composition, although the changes differed among the two cohorts, mainly due to differences in dietary intake.
Overall, the evidence suggests that fasting may be able to increase microbial richness and butyrate-producing bacteria in the short term, although fasting affects different people in unique ways, depending on age, dietary intake and ethnicity.
Whilst focussing on when you eat may offer some health benefits, we know that what you eat can shape your microbiome for the better.
Whether fasting or not, we recommend a Mediterranean-style diet rich in plant-based fibres like whole grains, legumes, nuts and a colourful variety of fruits and vegetables.
Not only is the Mediterranean diet linked to increased microbiome diversity, but it can also reduce your risk for cancer, heart disease, obesity and stroke.
☝TIP☝ It is recommended that you eat 30g of fibre daily, but the more you manage, the better!
Who should avoid intermittent fasting?

Whilst intermittent fasting may offer benefits for some individuals, it's not suitable for everyone and can pose health risks to certain demographics, among them:
1.) Type-1 diabetics
Diabetics are at an increased risk for hypoglycemia when fasting, a condition where blood sugar drops to dangerously low levels. Insulin and other diabetic medications increase this risk even further.
2.) Individuals with a history of eating disorders
Fasting has been linked with an increased risk for bulimia and binge eating disorder. As such, we recommend that those with a history of disordered eating should not attempt fasting regimes.
3.) Pregnant or lactating women
Pregnant women require extra calories whilst carrying and are advised to avoid any restrictive eating plans.
4.) Older adults
There is a dearth of research looking at how intermittent fasting affects older populations. What's more, fluctuations in blood sugar and energy levels could lead to falls, so we recommend against fasting in this demographic.
Article summary
- Animal and human research suggest intermittent fasting may be able to improve cardiovascular and metabolic health.
- It is hypothesised that metabolic reprogramming is the main mechanism behind these benefits, enhancing the bodies ability to repair oxidative damage to cells.
- Fasting-related weight loss and microbiome alterations have also been suggested as possible mechanisms for the benefits.
- Although the research is scarce, fasting appears to change microbiome composition and, in some cases, boost diversity. Multiple studies also reported an increase in butyrate-producing and mucus-eating bacteria; both considered beneficial.
- Age, diet and baseline microbiome composition appear to influence how fasting shapes the microbiome.
- Fasting may be able to help manage the symptoms of type-2 diabetes, although this should be overseen by a medical professional.
- Fasting is not suitable for pregnant or breastfeeding women, those with a history of eating disorders or type-1 diabetics.
- Fasting research mainly comprises small-scale, short-term studies on young/middle-aged cohorts. As such, it remains unclear how fasting impacts older populations.
☝️DISCLAIMER☝This article is for informational purposes only. It is not intended to constitute or be a substitute for professional medical advice, diagnosis, or treatment.