Bile acid malabsorption is a little-known condition, yet a 2014 study found that 1 in 3 people diagnosed with IBS-D and functional diarrhoea have bile acid malabsorption.
Bile is an acidic digestive juice that helps the body break down fats. Typically, the body reabsorbs the bile and recycles it. When it doesn’t, it causes a condition called bile acid malabsorption, with diarrhoea as the primary symptom.
Crohn’s disease, gallstones, coeliac disease, and other diseases of the digestive system may cause bile acid malabsorption. It can also disturb the delicate equilibrium of the gut microbiome in the colon. Find out the symptoms of bile acid malabsorption, how it is diagnosed, and how it is treated in this article.
☝️DISCLAIMER☝This article is for informational purposes only. It is not intended to constitute or be a substitute for professional medical advice, diagnosis, or treatment.
Table of contents
- What is bile?
- Bile acid malabsorption
- Causes of bile acid malabsorption
- Symptoms of bile acid malabsorption
- Bile acids and the gut microbiome
- Diagnosing bile acid malabsorption (tests)
- Treating bile acid malabsorption
What is bile?
Bile is essential for the digestion of fats. It is made by the liver and stored in the gallbladder, where it is released into the small intestine during digestion.
Bile acids are made from cholesterol, and they are vital for the absorption and transportation of fats, nutrients, and vitamins. Primary bile acids, like cholic acid and chenodeoxycholic acid, participate in a few critical processes:
- the breakdown and absorption of fats and fat-soluble vitamins
- the removal of waste products from the body that are secreted into bile
Bile acids are detergent molecules that perform two functions. One end of the molecule loves water while the other likes fat, grease, or dirt, making them perfect for emulsifying dietary fats. Emulsified fats have a greater surface area, which makes it easier for digestive enzymes to them break down.
What is bile acid malabsorption?
Around 95% of bile acids are reabsorbed in the ileum, the final part of the small intestine, and are restored back to the liver.
This cycle is known as enterohepatic circulation. When this cycle is disrupted, it causes bile acid malabsorption. This condition is also known as bile acid diarrhoea (BAD), and bile salt malabsorption.
In bile acid malabsorption, too much bile acid enters the colon, which causes the large intestine to release more water. The increase in fluids results in a faster transit time of waste through the gut and chronic watery diarrhoea.
Causes of bile acid malabsorption
There are three types of bile acid malabsorption, and many potential causes, most of which are linked to digestive diseases and conditions.
| Type 1 | Problems affecting the ileum (small intestine) where bile acid is reabsorbed, such as surgical removal of the ileum, Crohn’s disease, or cancer treatment. |
| Type 2 | Idiopathic – no known cause. |
| Type 3 | Caused by other diseases or conditions affecting the stomach or gut. Examples include removal of the gallbladder, chronic pancreatitis, coeliac disease, or small intestine bacterial overgrowth (SIBO). |
Gallstones, fatty liver disease, and bile acid diarrhoea
Bile acids are produced by the liver and stored in the gallbladder. A 2017 study that studied the files of 578 patients found that bile acid diarrhoea was associated with gallstones and fatty liver disease.
Research shows that the idiopathic form (type 2) of bile acid diarrhoea may be caused by low serum fibroblast growth factor 19 (FGF19), which impairs the normal bile acid cycle. There is also evidence of increased weight being associated with bile acid malabsorption and low FGF19 levels.
☝️Find out if you are genetically predisposed to gallstones with the Atlas DNA Test.
Crohn’s disease
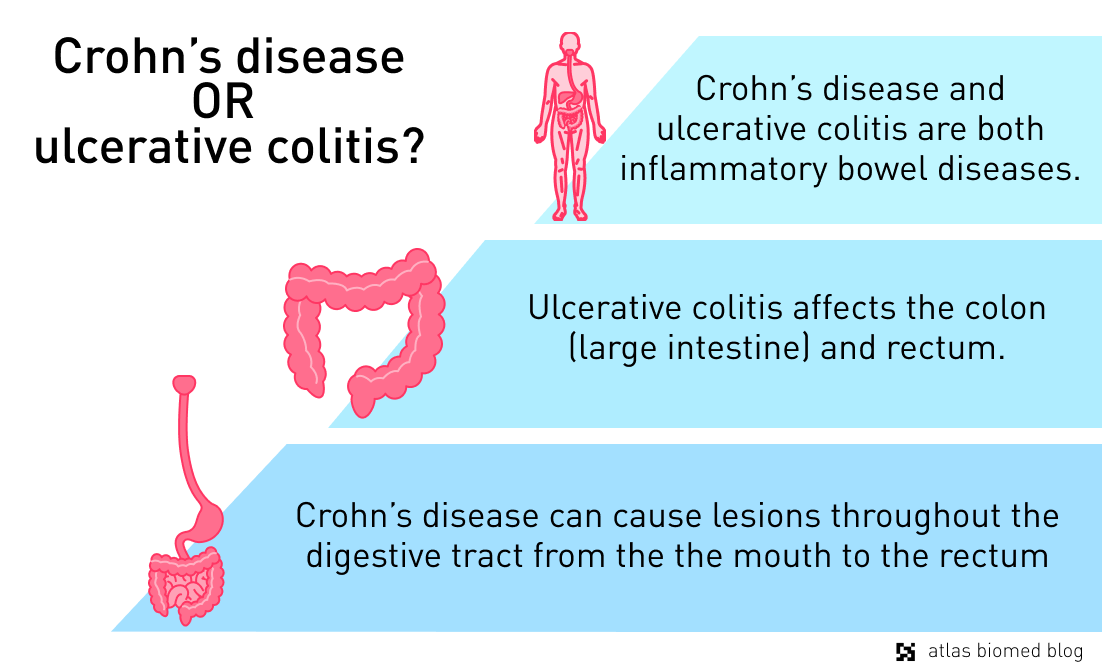
Bile acid malabsorption is a common sign of inflammatory bowel disease (IBD), especially Crohn’s disease. This serious lifelong condition can damage any area of the digestive tract lining from the mouth to the anus. Type 1 bile acid malabsorption is especially prevalent in people who have Crohn’s Disease and have experienced:
- ileal-resection (surgical removal of the ileum)
- ileitis (chronic inflammation of the ileum)
Discover whether you are genetically predisposed to inflammatory bowel disease and how your gut bacteria can influence your protection from this disease with the Atlas Microbiome Test.
Coeliac disease
Coeliac disease, a hereditary form of gluten intolerance, is an autoimmune condition in which gluten triggers the immune system, which starts to attack the cells in the small intestine. It causes many digestive-related symptoms including diarrhoea, constipation, weight loss, and pain.
Type 3 bile acid malabsorption affects coeliac patients because this disease can interfere with the bile acid reabsorption cycle. Coeliac disease also affects the absorption of nutrients, such as iron and zinc, when the digestive lining is inflamed.
☝Find out what your DNA and gut microbiome say about gluten intolerance with the Atlas Microbiome and DNA Tests.
Symptoms of bile acid malabsorption
The most common symptom of bile acid malabsorption is watery diarrhoea, which can also be present with or without steatorrhoea (excess fat in stools). Although the condition is not life-threatening, it can have a negative impact on an individual’s quality of life.
That’s because it causes an increased frequency of needing to go to the toilet which can dictate a person’s day-to-day life, and in severe cases, prevent them from leaving their home. Sometimes diarrhoea can be pale and greasy in appearance and may be difficult to flush.
Bile acid malabsorption symptoms
- watery diarrhoea - often yellow and greasy in appearance
- needing the toilet often
- bloating
- abdominal cramps
- excessive, smelly wind
Other symptoms can be similar to those of Irritable Bowel Syndrome (IBS), like bloating, excessive wind, and abdominal cramps. People who have bile acid malabsorption may also be at risk of vitamin B12 deficiency because the nutrient is absorbed in the ileum, the same place as bile acids.
So, if this section of the small bowel is damaged or diseased and vitamin B12 absorption is affected, it can cause symptoms like shortness of breath and feeling tired all the time. Therefore, in some people with bile acid malabsorption, fatigue may be a symptom. Bile acid malabsorption and joint pain are also reported by some patients.
Bile acids and the gut microbiome
The human gut is home to trillions of bacteria that help maintain a healthy colon, support immune health, and participate in metabolic processes. A balanced and diverse microbiome is associated with good health, but a fragile and unbalanced one is linked to many diseases.
In healthy people, small amounts of primary bile acids travel to the colon where specific gut bacteria transform them into secondary bile acids, like deoxycholic acid (DCA). These secondary bile acids regulate both the composition of the gut microbiome and the health of the host.
A 2020 study into the relationship between gut bacteria and bile acid diarrhoea found that patients with this condition had a less diverse microbiome. The authors also noted changes in short-chain fatty acid profiles and the composition of the gut microbiome. It is likely that, in the coming years, more will be known on this topic.
Bile acid malabsorption diagnosis
The gold standard bile acid malabsorption test is the selenium homotaurocholic acid test (SeHCAT). The patient takes a capsule containing radiolabeled bile acids and several images are taken at various time periods to monitor the bile acid cycle.
The test measures how many radiolabeled bile acids are still in the abdomen after several days. If the results show fewer radiolabeled bile acids, then it indicates that bile acids are not being retained normally, which is a sign of bile acid malabsorption.
Other diagnostic tests that may be used to diagnose bile acid malabsorption are serum biomarkers of bile acid synthesis in the liver, like fasting serum C4 and FGF19. Total and individual faecal bile acids may also be used.
Bile acid malabsorption treatment
The main treatment options available for bile acid malabsorption are medication and diet changes. Because type 1 and type 3 are caused by underlying health conditions, it may be necessary to treat them first, which may improve the symptoms associated with bile acid malabsorption.
Medication
Bile acid binders are prescribed to people who are affected by the malabsorption of bile acids. They work by binding to bile acids in the small intestine, preventing them from irritating the lining of the gut as they move through the gastrointestinal tract.
These fat reducing agents aren’t always well-tolerated. There is also a risk of gastrointestinal side effects like constipation, upset stomach, diarrhoea, and loss of appetite when taking them.
Low-fat diet
Individuals diagnosed with bile acid malabsorption may be referred to a dietician to help control their symptoms. In many cases, it is advised to eat less than 40g of fat per day and make healthy swaps, such as whole milk for skimmed or semi-skimmed varieties.
Bile acid malabsorption foods to avoid
- butter and margarine
- cream cheese
- fatty meats or meat with visible fat
- frying oil
- hard (full fat) cheese
- pastry (especially puff and shortcrust)
- skin on meat (e.g. chicken or pork crackling)
- whole milk
A 2015 study of 40 patients with bile acid malabsorption demonstrated that a low-fat diet could significantly reduce symptoms such as bloating, frequency of going to the toilet, and urgency. The participants also reported a reduction in gas, abdominal pain, and greasy poops.
Living with bile acid malabsorption
Bile acid malabsorption can have a severe impact on your quality of life, particularly if it is left undiagnosed or untreated. The most common symptom is diarrhoea, and some people may need to go in excess of 10 times per day.
This can significantly decrease a person’s quality of life and socialisation. Treatment such as medication or treating the underlying cause can help to relieve symptoms. Dietary changes may also be beneficial.
☝REMEMBER☝ If you suffer from prolonged diarrhoea, or severe gastrointestinal symptoms, don’t wait. Ask your doctor for help!