The vagus nerve is the body's most extensive and complex cranial nerve, linking the brain with all essential organs.
Not only is this communication highway an essential pathway in the gut-brain axis, but it also regulates our immune response and parasympathetic nervous system. Keep reading to learn six MINDBLOWING facts about the "wandering" nerve!
Table of contents
- The vagus nerve: the body's communication superhighway
- The gut-brain axis: brought to you by the vagus nerve
- Vagal stimulation can treat epileptic seizures
- Vagal stimulation may improve treatment-resistant depression
- Vagal damage can cause digestive issues
- Vagal overaction is the main cause of fainting
- Low vagal tone is associated with chronic inflammation
- Summary
The vagus nerve: the body's communication superhighway
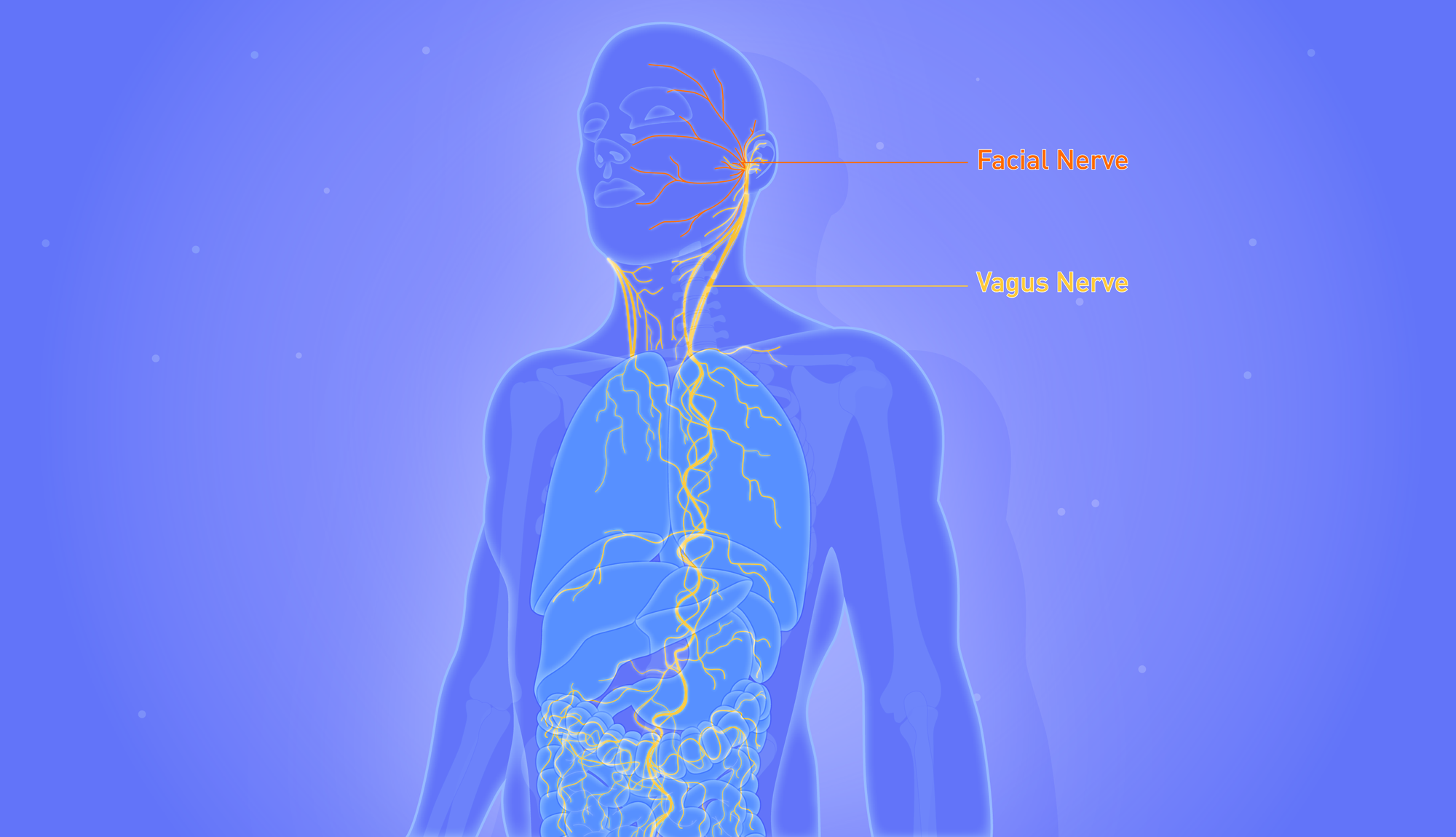
The vagus nerve is the longest and most complex of the cranial nerves, running from the brain stem to the abdomen and branching into numerous organs, including:
- heart
- lungs
- liver
- kidney
- stomach
- Large and small intestines
Whilst we talk about the vagus nerve in the singular, it comprises two parts- one traversing the left side of the body and another on the right.
Not only does the vagus nerve carry signals to our organs from the brain, but it relays sensory information back from the organs as well.
In fact, eighty per cent of vagus nerve fibres are efferent, meaning they can transfer sensory information to the brain stem from our organs, including the gut.
In Latin, vagus means wandering, a fitting name for this meandering nerve. It almost looks like a plant's root system, growing downwards from the brain.
When activated, the parasympathetic nervous system slows the heart rate and increases blood flow to the intestines, hence why it's also known as the "rest and digest" response. Think of it as an off-switch for the body's stress response.
As part of the parasympathetic system, the vagus nerve controls digestion, heart rate, swallowing and even your immune response.
As if that wasn't impressive enough, this multitalented nerve is responsible for regulating numerous reflex actions, such as coughing, sneezing, swallowing, and vomiting.
Moreover, emerging research suggests that vagal stimulation could help treat conditions as varied as depression, anxiety and inflammatory bowel disease.
Without further ado, let's take a look at six amazing facts about the vagus nerve- the body's super communication highway:
1.) The vagus nerve allows the gut to communicate with the brain and vice versa
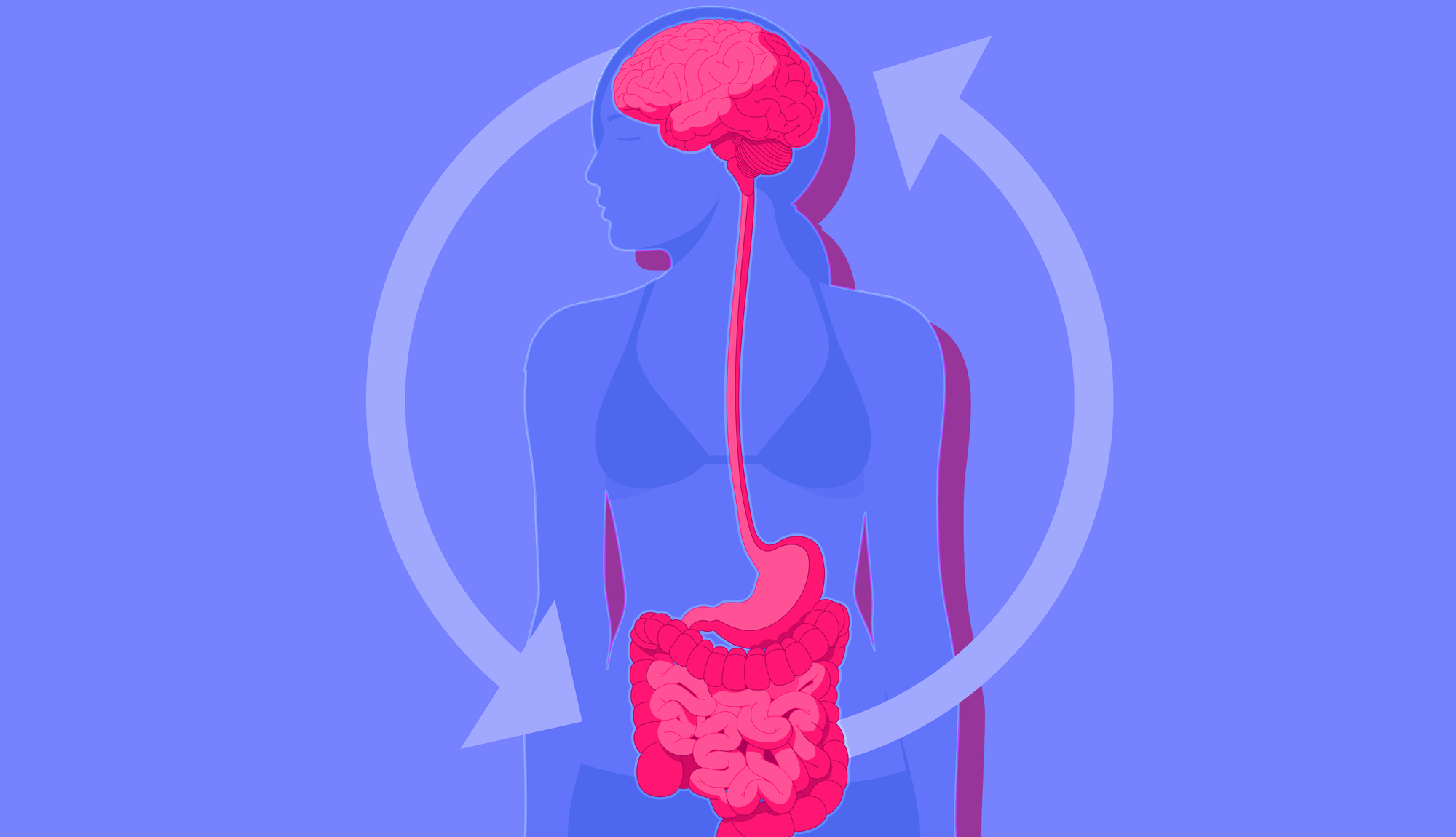
Believe it or not, your gut hosts a "second brain", known as the enteric nervous system. Made up of 100-500 million neurons, the ENS regulates digestive functions, including muscular contractions and fluid secretion.
The gut and brain may seem like odd bedfellows, but these two organs are intimately connected and chatter back and forth.
In short, the vagus nerve acts like a fibre optic cable, transmitting signals from the enteric nervous system to the central nervous system and vice versa.
Interestingly, most signals transmitted via the vagus nerve move in the gut-brain direction.
Believe it or not, the ENS can operate independently of the brain, making it the only organ in the body which can function autonomously.
How do we know this? When researchers severe the vagus nerve in mice, therefore cutting the phone line between the gut and brain, the gut continues to ripple away.
In other studies, cutting the vagus nerve can reverse behavioural changes triggered by microbiome transplants.
For example, mice translated with the microbiota of depressed donors exhibit increased despondency, called anhedonia.
Tellingly, this behaviour is reversed when the vagus nerve is cut, suggesting that the microbiome can influence mood via vagal transmissions. Neat, huh?
2.) Stimulating the vagus nerve can help reduce epileptic seizures
For those whose epilepsy does not respond to medication alone or those ineligible for brain surgery, Vagal Nerve Stimulation (VNS) therapy may help to minimise the frequency and severity of seizures.
VNS is a type of Bioelectronic medicine approved for use in those with treatment-resistant epilepsy by the FDA. It has been utilised as a treatment for epilepsy since the 1990s but remains in limited use.
VNS involves the surgical insertion of a device (generator) into the collarbone. The device is somewhat similar to a pacemaker, and the procedure only takes around 1-2 hours.
Next, a small wire is coiled around the left vagus nerve, and the generator is programmed to send regular, mild electrical signals to the brain via the vagus nerve.
While it may sound like something out of a horror film, the treatment is generally well-tolerated, with a hoarse voice, headaches and throat pain the most common side effects.
The effectiveness of the treatment varies widely across individuals, with some seeing drastic reductions in seizure severity/frequency, others mild changes and others no changes at all.
Researchers aren't entirely clear on how VNS can alleviate epilepsy, though it is thought that the electrical signals calm down irregular electrical brain activity. One way they may do this is by stimulating neurotransmitters that lower seizure activity.
Some patients also report an improvement in mood, memory and alertness, which leads us to our next point.
3.) Vagal Nerve Stimulation may be able to alleviate treatment-resistant depression
Soon after the FDA approved vagal nerve stimulation for treatment-resistant epilepsy, reports emerged of people experiencing improved mood as a byproduct of the procedure.
Some researchers sought to explore VNS as a potential treatment for chronic depression in light of these reports.
In one study, 200 individuals presenting with treatment-resistant depression were given vagal nerve stimulation.
In the first two months, no improvement was reported, but after one year, 20-30 per cent of the subject experienced drastic improvements, with half of these saying their symptoms were almost entirely resolved. With that said, others reported no improvement or even a worsening of their symptoms.
It is thought that VNS stimulates the production of feel-good neurotransmitters, redressing imbalances in depressed patients.
Moreover, a small-scale pilot study comprising 12 participants explored the use of VNS for treatment-resistant anxiety disorders.
Among the group, seven patients had a primary diagnosis of Obsessive-Compulsive Disorder (OCD), two had Post-Traumatic Stress Disorder (PTSD), and one had panic disorder (PD).
In general, VNS was well tolerated by the group, with some participants reporting acute and long-term symptom improvements.
We know that the vagus nerve sends signals to brain regions important in anxiety regulation, including the insula, hippocampus and amygdala, offering a potential mechanism for the benefits that were observed.
4.) An overreaction of the vagus nerve can cause fainting
If you have ever fainted at the sight of blood or getting an injection, the vagus nerve may well have been involved. Let me explain.
Fainting occurs when the brain receives insufficient blood for a short period of time. In some cases, an overreaction of the vagus nerve can cause you to lose consciousness, known as vasovagal syncope.
In short, certain stimuli can trigger an excessive parasympathetic response, drastically lowering blood pressure and heart rate.
As a result of these physiological changes, modulated by the vagus nerve, the brain receives insufficient blood.
A whopping eighty per cent of fainting events in those under forty are attributable to vasovagal syncope. Why this happens is up for debate, though one theory is that the body is preparing for trauma and trying to minimise blood loss.
5.) Damage to the vagus nerve can cause digestive issues

The vagus nerve can become damaged for various reasons, including stomach or oesophagal surgery and type-2 diabetes. Symptoms of damage include hoarseness of voice, a deficient gag reflex and difficulty swallowing.
Besides these symptoms, vagal damage can manifest itself through digestive issues. For example, vagal damage is known to cause gastroparesis, a chronic condition where the stomach cannot empty food properly.
If the wandering nerve is damaged, the signals triggering peristalsis can be disrupted, resulting in a long list of digestive woes, among them:
- bloating
- nausea
- cramping
- diarrhoea
6.) Low vagal tone is associated with chronic inflammation
Vagal tone refers to the strength of the signals transmitted by the vagus nerve. Interestingly, research has linked low vagal tone to chronic inflammation.
As we touched upon earlier, one of the vagus nerve's many jobs is to reset the immune system after a stress response, which it does by switching off the production of inflammatory proteins called Tumour Necrosis Factor (TNF).
However, in those with a low vagal tone, it is thought that the regulation of our immune response becomes impaired, leading to excessive inflammation.
Preliminary evidence suggests that vagal stimulation, which increases vagal tone, may be able to minimise inflammation and, more specifically, effectively treat rheumatoid arthritis.
In short, a Dutch study observed lower levels of TNF in the bloodstream of 7 epileptic patients when zapped with a vagal pacemaker. The bioelectric treatment also significantly reduced the production of two inflammatory cytokines, (IL)-6 and IL-1β.
In the second part of the study, the research team installed VNS devices in seventeen volunteers with rheumatoid arthritis.
After eighty-four days, the patients exhibited significantly reduced levels of inflammatory TNF in the bloodstream alongside drastic improvements in their symptoms. All of the subjects opted to keep their devices installed.
Summary
- The vagus nerve allows the brain to network with all our essential organs
- It is the primary nerve in the body's parasympathetic nervous system- the counterpart to the fight-or-flight stress response
- A damaged vagus nerve can cause gastroparesis, a condition where the stomach cannot properly evacuate food
- In some cases, Vagal Nerve Stimulation (VNS) can improve symptoms in those with treatment-resistant epilepsy and chronic depression
- Preliminary evidence suggests that VNS may be able to treat various conditions, including anxiety disorders and inflammatory diseases such as rheumatoid arthritis and Crohn's

☝️DISCLAIMER☝This article is for informational purposes only. It is not intended to constitute or be a substitute for professional medical advice, diagnosis, or treatment.