Take an in-depth look at some common diagnostic tests for digestive health, including which organs they can inspect, what diseases they can help diagnose and what each procedure entails.
Table of contents:
- The digestive organs
- What is a diagnostic test?
- Faecal tests
- Endoscopic procedures
- Breath tests
- Imaging tests
- Manometry tests
When digestive issues arise, be that bloating, pain, constipation or something else entirely, there are a range of methods doctors can use to eliminate possible causes and ultimately understand the source of your symptoms.
In this article, we are going to have a look at common diagnostic procedures employed by clinicians and what these tests look for.
The digestive organs
Before looking at the different diagnostic tests used to detect digestive issues, we are going back to school and looking at the organs which constitute the gastrointestinal tract.
Gastro what? More commonly known as the GI tract, it refers to the many organs which food passes through when it is swallowed, digested and absorbed into the body. These organs are connected by a long winding tube that runs from the mouth to the anus and includes:
- The Oesophagus
- Stomach
- Small intestine
- Large intestine
- Rectum
- Anus
These are supported by organs like the pancreas, liver and gallbladder. As you can tell, digestion involves far more than a stomach and the intestines! To understand this a bit better, let’s follow a meal on its journey through the human body and into the toilet bowl. It’s a hell of a ride:
Oesophagus
Once you have chewed your food and swallowed, your meal slides down your oesophagus and towards your stomach. The oesophagus moves food towards the stomach entry with a kind of Mexican wave of contractions, known as propulsive peristalsis.
The food then enters the stomach through the lower oesophagal sphincter which separates these two organs. In Gastroesophageal reflux disease (GERD), this ring-shaped muscle is weakened and relaxes when it should not, resulting in acid reflux.
Stomach
The stomach is like a big washing machine and physically throws the food around, breaking it down into a smoothie-like consistency with the help of enzymes and acid.
It is much higher up than people often assume, so when children complain of a tummy ache, they are likely rubbing the intestines instead. The mashed-up food, known as chyme, travels through the pyloric sphincter into the duodenum, the first part of the small intestine to me and you.
Small intestine
The small intestine is actually the longest part of our GI, measuring in at approximately 6m! It is covered in lots of finger-like structures called villi, increasing the surface area of the small bowel. These play a key role in nutrient absorption, and if damaged or flattened, as in undiagnosed celiac disease, can lead to nutrient deficiencies. These villi hash and push the chyme forward, drawing nutrients into its inner walls that are as thin as 1 cell thick!
The small intestine does not work alone and receives digestive enzymes from the pancreas and gallbladder, important players in the orchestra that is digestion. The liver processes nutrients absorbed in the small intestine, and also produces detergent-like bile to help digest fats and some vitamins.
Large intestine
After its journey through the small intestine, the chyme enters the large intestine through a structure known as Bauhin’s valve. The large intestine is about 1.5m long, but much wider than the small intestine, and is where the majority of your gut microbiome live.
What’s left of your dinner at this point is mainly undigested fibre that our human enzymes cannot break down. Our gut microbes kindly do this for us and get more nutrients from our food. Quick clarification, the large intestine is also known as the colon. It is broken down into 4 parts: The ascending colon, the transverse colon, the descending colon, and the sigmoid colon.
Rectum
The rectum begins at the end of the colon, called the sigmoid, and extends all the way to the anus. The rectum compacts and stores the waste products of digestion, which we know as poo, ready for expulsion.
☝Did you know?: Poo is made up of water, bacteria (both dead and alive), undigested fibre, bile and dead red blood cells. We sequence the DNA of this bacterium in the the Atlas Microbiome Test to discover the composition of your gut bacteria
Anus
This is the opening at the end of the rectum where faeces pass through. The anus has a ring of muscles known as the sphincter that keeps it closed between stool movements. There is both an internal and external sphincter. Damage to these can cause incontinence whilst improper contractions can lead to constipation.
Poo POV: follow your food on a journey from gums to bum
What’s a diagnostic test?
A diagnostic test is any procedure used to confirm or rule out suspected conditions. To reach a diagnosis, your doctor might ask you to undergo more than one diagnostic test. These tests can be invasive and non-invasive, simple and complex, but all of these diagnostic tests are crucial for identifying and treating conditions and learning more about symptoms.
If you are experiencing gastrointestinal issues, whether that be bloating, abdominal pain, trouble passing stool, difficulty swallowing or something else entirely, reach out to your GP as soon as possible.
These diagnostic tests are overwhelmingly safe and effective at identifying the cause of digestive issues, especially when combined. Whilst some may sound unpleasant, sedatives and anaesthetic mean you will not feel pain throughout. At most these can be uncomfortable, at best they can be lifesaving.
Below, we will look at some common diagnostic tests for digestive health, including which digestive organs they can inspect, what diseases they can help diagnose and what the procedures entail. The tests are broken down into five categories: Breath, Faecal, Imaging, Endoscopy and Manometry:

Faecal Tests
One way to examine the health of the digestive tract is to examine the waste products that it produces, or in other words, to analyse your poo.
Calprotectin test:
In this test, an individual will take a stool sample and send this off to a lab for testing where they will examine the levels of Calprotectin. This is a protein that is found in our white blood cells that has strong antibacterial properties and is central to our immune response.
When inflammation occurs in our intestines, calprotectin is released from activated white blood cells. As such, levels of this protein can be used as a diagnostic indicator of inflammatory bowel diseases such as Crohn's and ulcerative colitis. Patients might be required to provide multiple stool samples over a few days.
Occult blood test:
Occult blood simply means that it can’t be seen with the naked eye. In this faecal test, patients will submit a stool sample for analysis in order to see if there is any blood present. This procedure is used to determine whether there is bleeding in the GI tract, which could suggest bowel cancer and polyps in the rectum or colon.
Breath tests
Helicobacter pylori
If your doctor suspects you have an infection of H. pylori, a bacterium that infects the stomach causing ulcers, they might send you for a breath test. Patients referred for this test will have to abstain from eating shortly before the procedure.
During the test, the patient takes a small capsule with a substance called C13-urea inside. If H. pylori is present in the stomach, it will react with this substance producing gases detectable in the breath. The test takes around 30 minutes.
Hydrogen and methane breath test
A hydrogen breath test can be used to detect both lactose intolerance and small intestinal bacterial overgrowth (SIBO). Both tests require the patient to fast for up to 14 hours. In a test for lactose intolerance, individuals will be given a drink with a high-lactose content and asked to breathe into a device at intervals for around 2 hours. High amounts of hydrogen can indicate undigested sugars and as such, lactose intolerance.
In a SIBO breath test, patients will undergo the same process, however, the physician will measure levels of methane also. High levels of both gases are signs that bacteria has entered the small intestine and begun breaking down fibre too early.
This can be a valuable diagnostic test, although false negatives have been reported in some cases, namely because not all bacteria produce hydrogen when fermenting carbohydrates.
Endoscopic procedures
|
Name of endoscopic procedure |
Organ viewed |
Entrance point and method |
|
Gastroscopy |
Oesophagus, stomach and upper small intestine or duodenum |
A flexible tube is inserted through the mouth |
|
Capsule endoscopy |
Oesophagus, stomach, small intestine, large intestine, rectum |
A camera capsule is ingested through the mouth |
|
Flexible sigmoidoscopy |
The lower colon, or sigmoid |
A flexible tube is inserted through the anus |
|
Colonoscopy |
The entire large intestine |
A flexible tube is inserted through the anus |
|
Proctoscopy |
The rectum and anal cavity |
A tube is inserted through the anus |
|
Endoscopic retrograde cholangiopancreatography (ERCP) |
The liver, pancreas, gallbladder and bile duct |
An endoscope is inserted through the mouth |
There are many different types of endoscopy, but this table breaks down the method and subject of each one for you.
☝Did you know?: You might have heard people refer to the upper GI tract and lower GI tract. Quite simply, the mouth, oesophagus, stomach, and first part of the small intestine (duodenum) are known as the upper GI, whilst everything onwards is the lower GI tract
Gastroscopy
Also known as an esophagogastroduodenoscopy test, although I doubt any physician attempts to say it. This is used to diagnose conditions affecting the oesophagus, stomach and upper small intestine, such as:
- Gastroesophageal reflux disease (GERD)
- Coeliac disease
- Throat and stomach cancer
- Ulcers
- Barrett's oesophagus (damage to the tissue lining from acid reflux)
Before the procedure, patients are given a sedative and local anaesthetic. You will also be asked to fast for about 8 hours prior to the appointment. Once the sedative has taken effect, the doctor passes a small, flexible tube known as an endoscope down the throat, through the stomach and into the duodenum or upper small intestine, as we touched upon in biology 101.
This will have a camera and a light on it and will feed images to a screen for the doctor to study. Air is pumped into the stomach to inflate the organ and help the physician see better. A biopsy can be performed, which is when small bits of tissue are removed for testing.
Endoscopic retrograde cholangiopancreatography (ERCP)
This test combines a classic endoscopy with X-rays to examine bile ducts, the liver, gallbladder and pancreas. It can be used to diagnose blockages, infection or stones in the bile ducts, fluid leakage or narrowing of the pancreas and tumours.
After being given sedatives intravenously, a flexible, lighted tube, or endoscope, will be fed through to the duodenum as in a normal endoscopy. Once the scope is in place, a tube will be inserted through the scope and a contrast dye will be injected so your organs are visible on X-ray scans.

Wireless capsule endoscopy:
In this procedure, a small capsule with a camera inside is ingested and a sensor device is worn on a belt worn around the patient's waist; this allows the pill camera to transmit images from inside the stomach, up to 144,000 in an average test!
The footage being relayed is then analysed by a GI specialist to determine the next steps. Prior to this procedure, the patient will be required to fast and take laxatives to clear residual food debris.
Capsule endoscopy can be particularly helpful in diagnosing polyps, inflammatory bowel disease, ulcers, and tumours of the small intestine, large parts of which cannot be accessed by other endoscopic procedures. With that being said, it does not allow for tissue samples to be taken as in a colonoscopy or upper GI endoscopy.
As a result, if any abnormalities are spotted, a more invasive procedure might be required to investigate. In one study, capsule endoscopy was found to be more effective at spotting small growths than a CT scan, another minimally invasive procedure.
As it travels the whole length of the digestive tract, it can be used to detect issues in all of the organs from the oesophagus to the rectum.
Lights, camera, digestion! The video above gives an inside look at digestion through the use of capsule endoscopy.
Colonoscopy
A colonoscopy is a diagnostic test used to detect abnormalities in the large intestine, such as cancerous growths, inflammatory bowel diseases and polyps (non-cancerous growths that can turn cancerous). Unlike many other tests, it allows a physician to see the entire length of the large intestine.
Before the procedure, patients will have to avoid solid foods for around 1-3 days, and take a laxative shortly before the examination to clear out the intestines of food debris. A sedative is administered for the procedure so patients need to be monitored afterwards. During the test, a specialist doctor blows air into the colon through the rectum, thereby enabling them to see better.
They then use a device called a colonoscope, which is a flexible tube with a camera and light attached at the end, to observe the entire length of the large intestine. If necessary, they can painlessly take samples of tissue, called a biopsy. These can be tested for cancerous cells later.
Flexible sigmoidoscopy
This is similar to a colonoscopy, however, it is slightly less invasive, and is used to look at the lower portion of the colon only, called the sigmoid. A small flexible tube with a camera and light is inserted into the anus and fed through to the lower colon.
This can be used to detect polyps, cancerous growths and inflammatory diseases. A similar procedure called a proctoscopy or rigid sigmoidoscopy can be used to examine the rectum.
Imaging tests
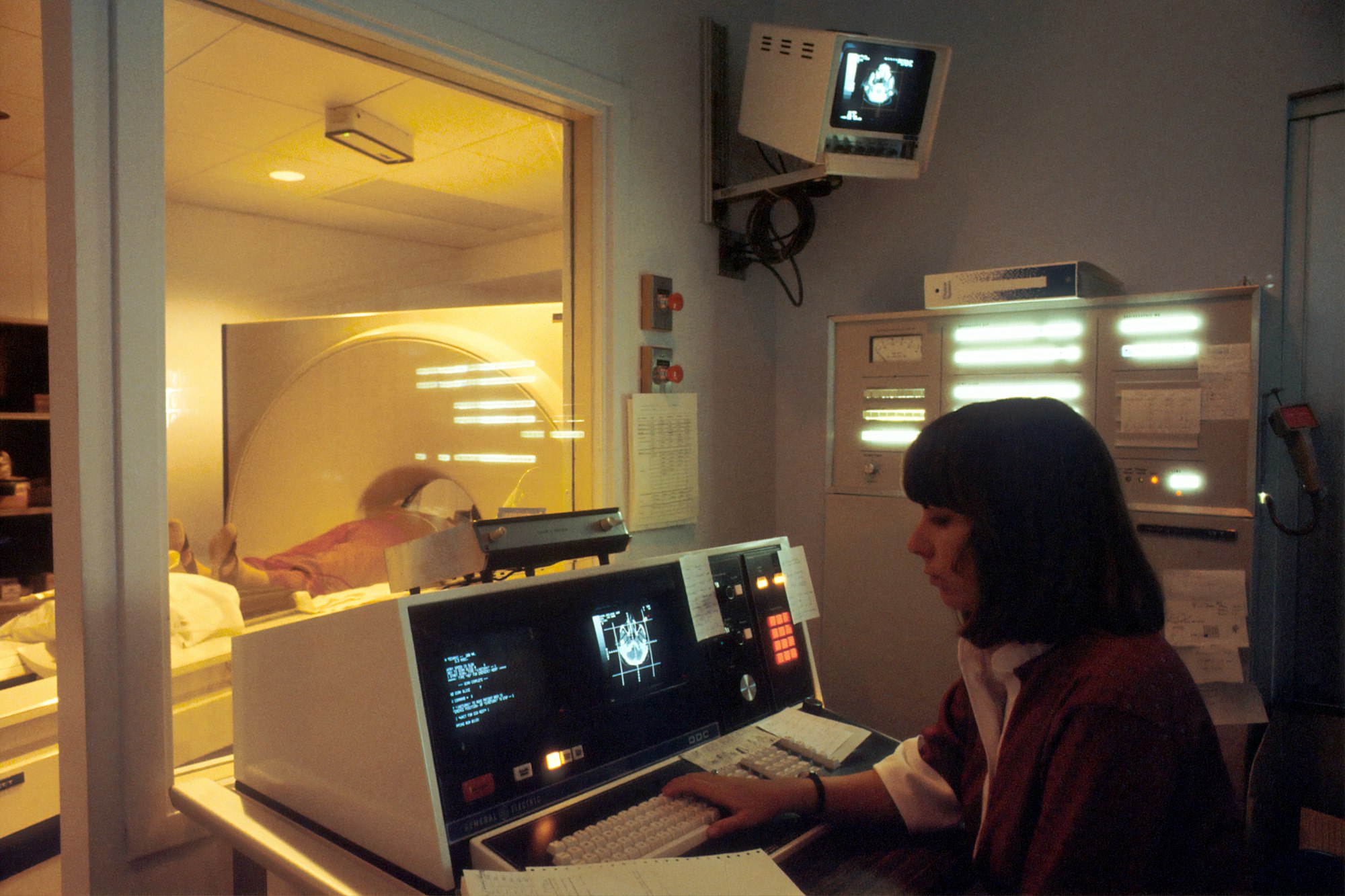
MRI scan
An MRI scan is a non-invasive test that can be deployed to examine the digestive organs; using powerful magnets and radio waves, it creates detailed, 3-dimensional images. It is an effective way to detect gastrointestinal problems such as:
- Appendicitis
- Inflammatory bowel diseases
- Acute pancreatitis
- Choledocholithiasis (when a gallstone blocks bile ducts, affecting digestion)
MRI scans are a safe procedure and there should not be any complications, but it can be claustrophobic and loud in the scanner, so a sedative might be administered if necessary. Alternatively, you might be able to listen to music to relax with the doctor's permission.
CT colonography (virtual colonoscopy)
A computerised tomographic (CT) colonography, commonly called a virtual colonoscopy, uses a series of X-rays to build a picture of the large intestine. It is particularly useful for detecting benign polyps and cancerous growths. Alongside a colonoscopy, it can also be used to detect Diverticular disease, where small bulges form in the large intestine causing pain. A lack of dietary fibre can increase the chances of developing this.
During the procedure, a small tube is inserted into the colon via the anus and inflates it with air. The patient then enters a tunnel-shaped device where X-rays are taken from multiple angles. These images are then used to construct a 3-dimensional view of the intestine.
The 3D images can allow the doctor to view parts of the intestine that might be obscured in a standard colonoscopy, however, a CT scan can be less effective at spotting small polyps. The night before the test the patient will likely be asked to drink a fluid that helps highlight the intestinal tract better.
Barium swallow and barium meal tests
This test uses X-rays and a substance called barium which coats the GI tract and makes it visible to a radiologist. There are multiple types of barium tests that can be performed: firstly, there is the barium swallow, which is used to look for abnormalities in the oesophagus and upper stomach, such as ulcers, growths and blockages.
Secondly, there is the barium meal, used to observe the oesophagus, stomach and beginning of the small intestine, called the duodenum. Lastly, those with gastrointestinal symptoms can also have a barium enema, which allows a doctor to observe the colon in an X-ray.
These tests allow a physician to examine the shape of the GI tract and determine how quickly food is moving through it. These tests might be performed for a variety of reasons, such as difficulty swallowing, unexplained vomiting, abdominal pain and bloody stool.
Manometry
Oesophageal manometry
If someone is suffering from persistent heartburn or pain and difficulty when swallowing, a physician might order an oesophageal manometry to test the strength and coordination of muscle contractions when they swallow. Remember the Mexican wave we discussed earlier in biology 101, called peristalsis?
This test can be used to eliminate conditions that mimic the symptoms of Gastroesophageal Reflux Disease (GERD), thereby aiding in a diagnosis. It is often used to decide whether someone is suitable for GERD surgery.
During the procedure, a small tube is inserted into the nose (local anaesthetic is applied) and passed through the throat into the oesophagus. The tube picks up vibrations from the muscle contractions, which are then graphed onto a machine.
Anorectal manometry
This test measures how well the anal sphincter and rectum are working and is often undertaken when someone is suffering from either faecal incontinence or constipation. A catheter with a deflated balloon is inserted via the anus, into the rectum.
The balloon is then slowly inflated, triggering contractions, which are measured via a machine connected to the catheter. This test helps a physician to see how the anal sphincter muscles are working, and whether these are weakened, damaged or improperly contracting.
Be proactive
Diagnostic tests can help medical professionals determine what is causing digestive symptoms and to choose the most effective treatment plan. Especially when combined, these tests are invaluable tools for identifying abnormalities and preventing complications.
If you or a loved one are experiencing digestive difficulties, regardless of your age, consult your GP and discuss this as soon as possible. Those 60 and over are eligible for colon cancer screening every two years on the NHS, but anyone at average risk or above of these complications should get screened regularly beyond the age of 45. Be proactive about your digestive health and don't wait for a crisis.
☝️DISCLAIMER☝This article is for informational purposes only. It is not intended to constitute or be a substitute for professional medical advice, diagnosis, or treatment.