Obesity, diabetes type 2, and coronary heart disease are metabolic illnesses influenced by the activities of your gut microbiome. Here’s what you need to know.
At a glance, these types of chronic diseases may seem different, but they are all the result of disruptions to the body’s metabolism. The term “metabolism” refers to all the chemical reactions in your body.
In many ways, the human body is much like an engine - it’s just much more complex, and far more advanced than any motor ever built. Even small changes in the body’s metabolism can affect our health.
Metabolic processes turn food into energy to fuel our cells, extract the building blocks for our working parts (proteins, fats, and nucleic acids), and help eliminate waste products from the body. So when they are disrupted, illness may ensue.
You are not alone if you can’t see the link between obesity, diabetes, and heart disease - let alone how microscopic organisms are involved. However, these three chronic diseases have a lot in common when you dig into the minutiae of human metabolism.
Obesity, coronary heart disease, and diabetes type 2 are intimately linked, and having one increases the risk of the other two, so much so that the medical community is considering putting them under the same umbrella.
This article explains more about these diseases, and how the gut microbiome can protect from them. We also review lifestyle risk factors and why eating a diet high in prebiotics (present in whole plant foods) can help.
Coronary heart disease
| Coronary Heart Disease | Go to my disease risk report now |
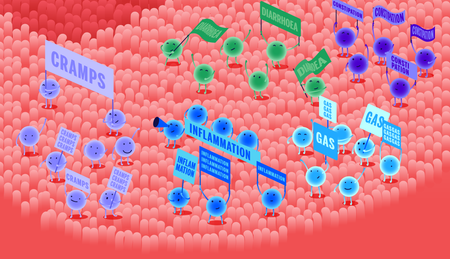
Coronary heart disease (CHD) is characterised by inflammation and plaque build-up on the blood vessel walls (atherosclerosis) that supply the heart - these deposits are made up of cholesterol. They progressively narrow the coronary arteries and may eventually completely block them.
When plaque grows enough to obstruct the passage of blood through the vessel, it causes blockages which lead to heart attacks. It is a primary cause of cardiovascular disease. According to a 2015 study, atherosclerotic cardiovascular disease is the leading cause of mortality worldwide.
Genetics can increase the risk of this disease: some people may have gene variants that influence blood cholesterol metabolism. Moreover, dietary choices also carry important risk burden, such as added sugars in processed foods and soft drinks, as well as the saturated and trans fat content of ready-made meals and snacks.
Specific changes and negative patterns in the gut microbiome, what researchers call dysbiosis, have been linked to increased risk of CHD because beneficial bacteria are less abundant and less desirable species are more common.
Beneficial bacteria help protect us from disease by their activities, which have positive benefits for the whole body. For example, at healthy levels, Akkermansia muciniphila has been shown to diminish the atherosclerotic lesions by maintaining the gut lining and preventing toxins from passing into the bloodstream and causing inflammation.
In a similar manner, Roseburia inulinovorans, Faecalibacterium prausnitzii, and Eubacterium rectale are also important because they produce butyrate, an essential short-chain fatty acid that protects against inflammation and support the integrity of the gut lining.
These markers include elevated representation of Proteus, Edwardsiella, and Providencia in the gut microbiome. They can produce trimethylamine (TMA) from choline (found in egg yolks) and L-carnitine (found in red meat and fish).
TMA is absorbed by the liver and oxidised into trimethylamine-N-oxide (TMAO), a compound associated with higher risk of atherosclerosis and coronary heart disease.
Developing coronary heart disease is a significant risk for people with type 2 diabetes, and many of these patients will succumb to this disease as a consequence. At the same time, obesity is considered a major risk factor in the development of coronary heart disease.
By identifying patterns and specific features of the gut microbiome in coronary heart disease, it is possible to evaluate how well your bacteria protect you from it with the Atlas Microbiome Test.
Diabetes type 2
| DIABETES TYPE 2 | Go to my disease risk report now |
Type 2 diabetes mellitus (T2D) is a metabolic disease in which the body’s insulin response doesn’t work properly, leaving high levels of glucose to circulate in the bloodstream with serious consequences for the body.
In healthy individuals, insulin is a hormone that signals the liver, muscles, and fat cells when it’s time to take in glucose and store it for energy. When the insulin response is blunted, glucose stays in the blood and damages the vessels that deliver blood to your organs.
Obesity and overweight, lack of exercise, and working nights are significant risk factors for diabetes type 2. While the exact mechanics are not always clear, these factors are linked to insulin resistance, which makes the liver, muscles, and fat cells less responsive to this hormone.
However, studies have also pinpointed an important link between the composition of the gut microbiome and diabetes type 2. As with coronary heart disease, beneficial species of bacteria are less abundant in the gut of patients with this disease compared to healthy people.
Studies show that healthy people have higher levels of butyrate-producing bacteria like E. rectale, F. prausnitzii, Roseburia intestinalis, and R. inulinivorans compared to patients with T2D. These bacteria feed on dietary fibers present in whole foods to produce butyrate, which has important anti-inflammatory functions.
This may help explain the link between the Western diet, which is high in refined sugars, fats, and animal products, and doesn’t contain enough plant-based foods. The fibers in these types of foods are called prebiotics because they encourage the growth of beneficial bacteria that support human health.
As previously mentioned, coronary heart disease is a common cause of mortality in patients with type 2 diabetes. Obesity is a strong factor in the emergence of this metabolic disease too: the degree of obesity and where the fat deposits accumulate are important predictors of T2D.
By identifying patterns and specific features of the gut microbiome in diabetes type 2, it is possible to evaluate how well your bacteria protect you from it with the Atlas Microbiome Test.
Obesity
| OBESITY | Go to my disease risk report now |
Obesity is defined by excess fat deposits in the body, either in specific places or all over, that increase a person’s risk of developing other illnesses, like diabetes type 2 and cardiovascular disease.
The gut microbiota also has an important role to play in the emergence of obesity, and growing research indicates that bacteria are involved in weight gain, may stimulate or decrease the hunger response, and can even protect from this disease.
The associations between obesity and the activities of gut bacteria were particularly well highlighted in a recent case. A woman of normal body weight had an infection called C diff and she was treated with a new and effective method: a faecal microbiota transplant (FMT - aka “poop transplant”) to repopulate her microbiome with healthy bacteria.
Shortly afterwards, she gained a lot of weight very quickly and doctors felt compelled to investigate. They discovered that she had received a stool transplant from an obese donor, and even though it treated her infection, it gave her microbiome specific traits that influenced her body mass significantly.
Gut bacteria influence many metabolic parameters linked to body mass. Depending on the composition of the gut microbiome, microbes may extract more or less energy from food and have an impact on how the body breaks down and stores fat.
Photo by Christopher Flowers / Unsplash
What you eat has a major impact on your health and disease risks
In addition to that, these bacteria even influence the endocrine system, which is responsible for metabolism, growth, hunger and satiety, as well as many other functions like mood, sexual reproduction, and sleep.
The gut microbiota of obese patients is characterised by low diversity, which means there are not enough different types of bacteria in the gut. At the same time, science shows that the bacteria present are better at extracting energy from food, increasing the energy available to the body (which is then stored in fat cells).
Akkermansia muciniphila and Christensenella minuta are known to protect against obesity. In particular, A. muciniphila is associated with lean body mass and protects against metabolic disorders and insulin resistance.
Beneficial butyrate-producing bacteria like Roseburia sp. and E. rectale tend to be more abundant in healthy people, compared to those with obesity. This is probably because such bacteria thrive on dietary fiber, of which there is not enough in their diet.
Evidence suggests that fiber is an important factor both for health and the composition of the gut microbiota. By adding more whole foods that are natural sources of dietary fiber to the diet, it has a knock-on effect for the bacteria in the gut, promoting the existence of those with health-promoting attributes.
By identifying patterns and specific features of the gut microbiome in obesity, it is possible to evaluate how well your bacteria protect you from it with the Atlas Microbiome Test.
What next?
It’s now possible to quantify your risk status for these metabolic diseases using DNA genotyping and comprehensive lifestyle questionnaires, combined with gut microbiome testing.
It also comes with personalised food, lifestyle, and probiotic recommendations designed to lower your disease risk and improve your protection against these common, chronic, and serious diseases.
- NJ Temple Fat, Sugar, Whole Grains and Heart Disease: 50 Years of Confusion, 2018
- S Barquera et al., Global Overview of the Epidemiology of Atherosclerotic Cardiovascular Disease, 2015
- AL Johnsson & F Backhed, Role of gut microbiota in atherosclerosis, 2017
- FH Karlsson et al., Symptomatic atherosclerosis is associated with an altered gut metagenome, 2012
- J Zhuye, The gut microbiome in atherosclerotic cardiovascular disease, 2017
- J Li et al., Akkermansia Muciniphila Protects Against Atherosclerosis by Preventing Metabolic Endotoxemia-Induced Inflammation in Apoe-/- Mice, 2016
- J Qin et al., A metagenome-wide association study of gut microbiota in type 2 diabetes, 2012
- RH Eckel, Obesity and Type 2 Diabetes: What Can Be Unified and What Needs to Be Individualized?, 2011
- JQ Purnell M.D., Definitions, Classification, and Epidemiology of Obesity, 2018
- M Blaut & S Klaus, Intestinal Microbiota and Obesity, 2011