Gut bacteria can help alleviate stress, anxiety and depression, but they can also make it worse. Here are the facts on mental health and the microbiome.
Your gut microbiome is a collection of trillions of bacterial cells located largely in the colon. This organ is not only responsible for letting nutrients into the body, it’s also directly connected to the brain.
Researchers have been investigating how bacteria in your colon influence health by interacting with the immune system, strengthening the gut barrier, and preventing inflammation. Now we know that these activities also affect our mood, anxiety levels, stress resilience, and depression.
When the body experiences stress, it causes a cascade of events that are designed to help us escape imminent danger. It shuts down non-essential activities like sexual desire, reproduction and digestion, and uses chemical messengers to direct its resources and energy to the brain and muscles. This has repercussions for the gut microbiome too.
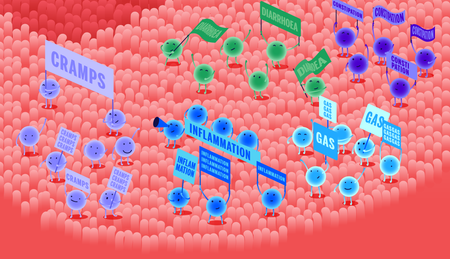
An unbalanced gut microbiome has negative consequences for your mood
A lesser known fact is that an unbalanced gut microbiome has consequences for your mood because bacteria can also influence anxiety and stress by their activities in the gut. They can play a positive role by enhancing our resilience to stressful events, but if the ecosystem is not balanced (something scientists call dysbiosis), their activities can have a negative impact on our mental health.
In this article, the newest member of our Board of Scientific Advisors, clinical neuroscientist and nutritionist Miguel Toribio-Mateas weighs in on these important functions. His speciality? Gut-brain communication.
| The gut-brain highway | The microbiome communicates with the brain using the vagus nerve. |
| Butyrate and inflammation | Inflammation can contribute to depression and gut bacteria can influence inflammation. |
| Probiotic bacteria | Research shows that probiotic gut bacteria can alleviate depression and anxiety. |
| Neurotransmitters and the microbiome | Gut microbes have an impact on the production of mood-promoting and calming compounds. |
1. The gut-brain highway
The gut and the brain are directly connected by the vagus nerve. The what? Before you run for the hills, stay a while and read, we promise to keep it simple.
The vagus nerve plays an important role in the autonomic nervous system: this is what allows you to breathe, swallow, and digest without thinking about it. This nerve is made up of fibers that connect the brainstem to the digestive organs, where they are embedded in the lining of our digestive organs (the epithelium).
By doing so, the vagus nerve participates in motility (the muscle movements that push food through the gastrointestinal tract), secretions of digestive substances, and food intake (feeling hungry or full). It can also tell the brain to release anti-inflammatory substances in response to digestive inflammation, and shut down the permeability of the gut lining.
When gut bacteria break down food particles, they produce metabolites, like butyrate (more on this essential short-chain fatty acid below), that can be sensed by the vagus nerve. In turn, this nerve transmits this data to the brain, which regulates digestive processes.
But stress shuts down the vagus nerve, preventing it from performing these important tasks. If the vagus nerve is unresponsive due to stress, it can’t release anti-inflammatory molecules that appease inflammation. Gut microbes are sensitive to stress and inflammation, and the ecosystem may suffer as a result.
Expert Miguel Toribio-Mateas says
Stress can lead to changes in both the numbers (abundance) and types (diversity) of bacteria. This can have a knock-on effect for mood via the gut-brain communication system known as the hypothalamic-pituitary-adrenal (HPA) axis.
This system includes your adrenal glands, the vagus nerve, and the brain's limbic system, which itself features the amygdala, often quoted as the part of the brain that rules the “fight or flight” response.
Communication between gut and brain is bidirectional, but messages sent from the gut to the brain are much stronger than those from the brain down.
As a very rough guide, the calmer and more balanced things are in the gut, (i.e. good intestinal barrier integrity, good diversity of bugs, lower inflammation, etc.), the more positive mental health outcomes tend to be.
2. Butyrate, inflammation and the gut lining
A balanced gut microbiome can strengthen the gut lining and protect from inflammation. By doing so, it plays a role in our mental wellbeing.
The gut microbiome needs to meet a few criteria in order for it to support our health. There should be an abundance of diverse microbes: this helps deter opportunistic bacteria that can make us sick, but it also means that the ecosystem is more resilient if something bad happens (like an infection).
A diversified microbiome has more bacteria that produce butyrate, a short-chain fatty acid that makes the gut lining less porous. In tandem with the vagus nerve, this activity helps prevent metabolites produced by microbes from reaching the brain where they can modify mood and anxiety levels.
When the gut microbiome suffers from dysbiosis, it means that balance and stability have been lost. This can be caused by a lack of diverse species, or when there are too many of some microbes, and not enough of others. It is also linked to lower production of butyrate and other important nutrients.
Inflammation affects the central nervous system and it can cause symptoms of depression. Conversely, depression can also cause inflammation. A diverse microbiome can help control inflammation through the production of butyrate because it strengthens the gut lining and prevents unwanted metabolites, toxins, and food particles from entering the body.
Expert Miguel Toribio-Mateas says
A widely accepted explanation says that intestinal permeability (aka “leaky gut”) occurs alongside chronic low-grade inflammation, which happens more often in disorders such as anxiety or depression.
Then it makes more sense to think that some bacteria like Lactobacillus rhamnosus or Lactobacillus farciminis have the ability to lower the increase of stress hormones (mostly cortisol and its derivatives, like cortisone) caused by stress.
There is still debate among scientists on the fine details of how these bugs manage to dampen the effects of neuroinflammatory changes induced by stress. What we do know is that their presence often results in a beneficial effect on the mucosal barrier (of the gut lining), and this then translates into more balanced mood.
3. Probiotic gut bacteria
Probiotics are not just supplements. Probiotic bacteria actually live in the gut microbiome and have science-backed benefits for mental health.
Species of Bifidobacterium, Lactobacillus (lactic acid bacteria), and Lactococcus are found in the colon where they exert a positive influence on whole body health, including anxiety and stress. This is because probiotic bacteria support the general well-being of a happy gut microbiome.
They produce important short-chain fatty acids and other substances that nourish the body, but also other species of beneficial bacteria. For example, Bifidobacteria produce acetate (a short-chain fatty acid) that feeds Eubacterium, who make butyrate from it.
Research into the effects of probiotic microbes on mental health, a field called psychobiotics, has also shown that species of Lactobacillus help improve our stress resilience and alleviate anxiety, memory, and cognitive symptoms. These include L. paracasei, L. acidophilus, L. plantarum, L. fermentum, and L. rhamnosus.
Some of them are found in the human gut microbiome, others in fermented foods like yoghurt and kefir, and some are found in both. The abundance of probiotic microbes in the gut can be improved by simple additions to your daily diet.
Supplementing the gut with prebiotic fibers found in whole foods like vegetables, fruit, grains, and legumes can encourage their growth in the gut microbiome. Traditionally fermented foods (unpasteurised) can also deliver probiotic bacteria to the ecosystem.
Expert Miguel Toribio-Mateas says
Some scientists have attributed psychobiotic properties to certain bacteria, on the basis of their ability to contribute to changes in psychological wellbeing.
This area is still very green and relies heavily on animal studies. For me, the biggest difficulty in the study of psychobiotics is that they are a food supplement, and people will take them as part of their daily life.
In real life conditions (not in the context of a clinical trial that is artificially isolated from reality to “keep things easy”), people eat different foods, do different types of exercise, and will engage in various behaviours (smoking, etc.). These all have consequences for microbiome and mental health.
My field of research is “real world evidence”. This means studying how a psychobiotic product works “in the real world”, taking into account all of these additional factors. This is an exciting way to look at the effects of psychobiotics, but it requires a lot of data over a longer time to gain any insights from it.
I believe in the next 5 years, we will know a lot more precisely how to use these psychobiotic bugs to help us with our mental wellbeing. In the meantime, I am tempted to recommend that people find natural sources of psychobiotics, like kefir, as opposed to relying solely on a food supplement. A specialist practitioner should be able to advise you on how to individualise this guideline.
4. Serotonin and GABA
Gut bacteria produce and regulate important substances for mental health, like serotonin (the happy hormone) and GABA.
Serotonin is a neurotransmitter (or a hormone, depending on who you ask) that influences many aspects of your physiology. When your body has enough serotonin, it helps regulate mood, happiness, and anxiety. However, low serotonin levels are linked to depression.
The gut microbiome makes happy chemicals for your body
Serotonin facilitates communication between the brain and cells of the nervous system. It’s also involved in many other processes too, like regulating bowel movements, sleep, nausea, and bone health.
Short-chain fatty acids produced by gut bacteria interact with the cells responsible for serotonin production in the gut. When the gut microbiota produces enough short-chain fatty acids, it actually promotes the production of serotonin.
It is important to remember that serotonin can be found in both the gut and the brain, but that gut serotonin cannot find its way into the brain because it cannot travel through the blood-brain barrier.
Gamma-Aminobutyric Acid, referred to as GABA, is a lesser-known neurotransmitter, but research indicates that it plays a role in regulating and improving mood. Strong emotional responses excite the nervous system, and this is where GABA comes in: it acts as a relaxant by counteracting the effects of excessive stimulation.
Gut microbes can also influence GABA, but rather than influencing the work of our cells, several strains of probiotic bacteria (Bifidobacterium, Lactobacillus, Lactococcus) can actually make GABA. Some bacteria also make a precursor molecule that the body uses to make GABA, called glutamic acid.
The gut has receptors and transporter proteins that allow GABA to cross into the body where its relaxant properties influence the central nervous system and brain.
Expert Miguel Toribio-Mateas says
We used to think that what happened in the gut stayed in the gut and, in many respects, scientific evidence seems to be confirming the exact opposite. It’s difficult to provide general advice on neurotransmitters and you go about managing them from the gut up because they all behave in different ways. But you can’t go wrong eating a variety of different foods, cooked in different ways, so as to feed into the diversity that is required by your gut ecosystem.
Your gut is like a meadow: you need to keep it fertile and balanced with plenty of different types of "flowers". For those who’d like to read more about this, I recommend a 2018 review by Briguglio et al., published in the journal Nutrients: Dietary Neurotransmitters: A Narrative Review on Current Knowledge.
It’s an open-access article (free to read) with wonderful illustrations on foods that contain different types of natural substances able to contribute to the generation of neurotransmitters facilitated by your gut bacteria.
What now?
The scope and impact of your microbiome reaches far beyond its home in the colon. These bacteria interact with us at many levels by mediating inflammation and producing important substances. Their activities even allow them to communicate with the brain via the central nervous system.
Vegetables, fruit, nuts, seeds, and legumes contain prebiotic substances, like dietary fiber, resistant starches, and other complex carbohydrates that fuel their activities and help maintain balance in the ecosystem. Simply put, prebiotics support beneficial activities, and by doing so, they can have a positive impact on your frame of mind.
Expert Miguel Toribio-Mateas says
Einstein is quoted to have said “Everything should be made as simple as possible, but not simpler.” The complexity of the microbiome is such that there are 2 extreme approaches.
One is to go to town and investigate every single bug (trying to help them grow or to reduce them), or focus on intestinal permeability with food supplements, or try to “tweak pathways” up and down. But there are still many unknown factors, and for someone who's not a scientist, it can be a bit too much.
The other extreme is to just do nothing much about gut health, on the basis that of “everything in moderation is fine”. The middle ground for me is a simple, science-based approach that tells us to go for around 30 plant foods per week.
If every week you aim to have 4 pieces of vegetables or fruit that are different to those you had last week, you’re nearly there. Mix and match, focus on different types of fibres, but also on colours.
Keep it bright and, of course, tasty. Enjoy your food and do not demonise any one food or food group unnecessarily. In my own years of practice, that has given the best results, so I’m quite happy with that level of science-based simplicity. Have a wonderful week!
- VA Pavlov et al., The Cholinergic Anti-inflammatory Pathway: A Missing Link in Neuroimmunomodulation, 2003
- CR Martin et al., The Brain-Gut-Microbiome Axis, 2018
- S Bright et al., Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders, 2018
- JD Forbes et al., A comparative study of the gut microbiota in immune-mediated inflammatory diseases—does a common dysbiosis exist?, 2018
- B Bonaz, The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis, 2018
- LC Lew et al., Probiotic Lactobacillus plantarum P8 alleviated stress and anxiety while enhancing memory and cognition in stressed adults: A randomised, double-blind, placebo-controlled study, 2018
- TG Dynan et al., Psychobiotics: A Novel Class of Psychotropic, 2013
- CJK Wallace at al., The effects of probiotics on depressive symptoms in humans: a systematic review, 2017
- Hormone Health Network, What is serotonin?
- S Liang et al., Recognizing Depression from the Microbiota–Gut–Brain Axis, 2018
- P Nuss, Anxiety disorders and GABA neurotransmission: a disturbance of modulation, 2015
- R Mazzoli & E Pessione,The Neuro-endocrinological Role of Microbial Glutamate and GABA Signaling, 2016
- CS Reigstad et al, Gut microbes promote colonic serotonin production through an effect of short-chain fatty acids on enterochromaffin cells, 2014
- A Farzi et al., Gut Microbiota and the Neuroendocrine System, 2018
- JA Foster et al., Stress & the gut-brain axis: Regulation by the microbiome, 2017